CerebraCell Technology
CerebraCell is targeting these disease states and conditions:
- Cerebral stroke recovery.
- Concussion recovery.
- Injury related brain damage.
- Brain cancer recovery.
- Parkinson’s.
- Alzheimer’s and dementia.
- Cerebral aneurysm repair.
- Depression.
- Brain memory recovery and enhancement.
- Brain function enhancement.
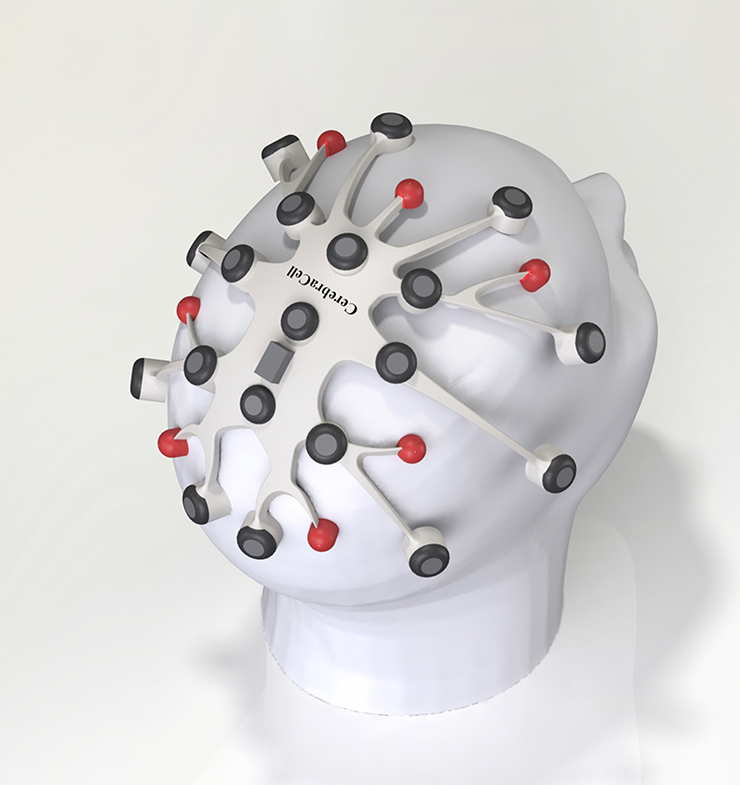
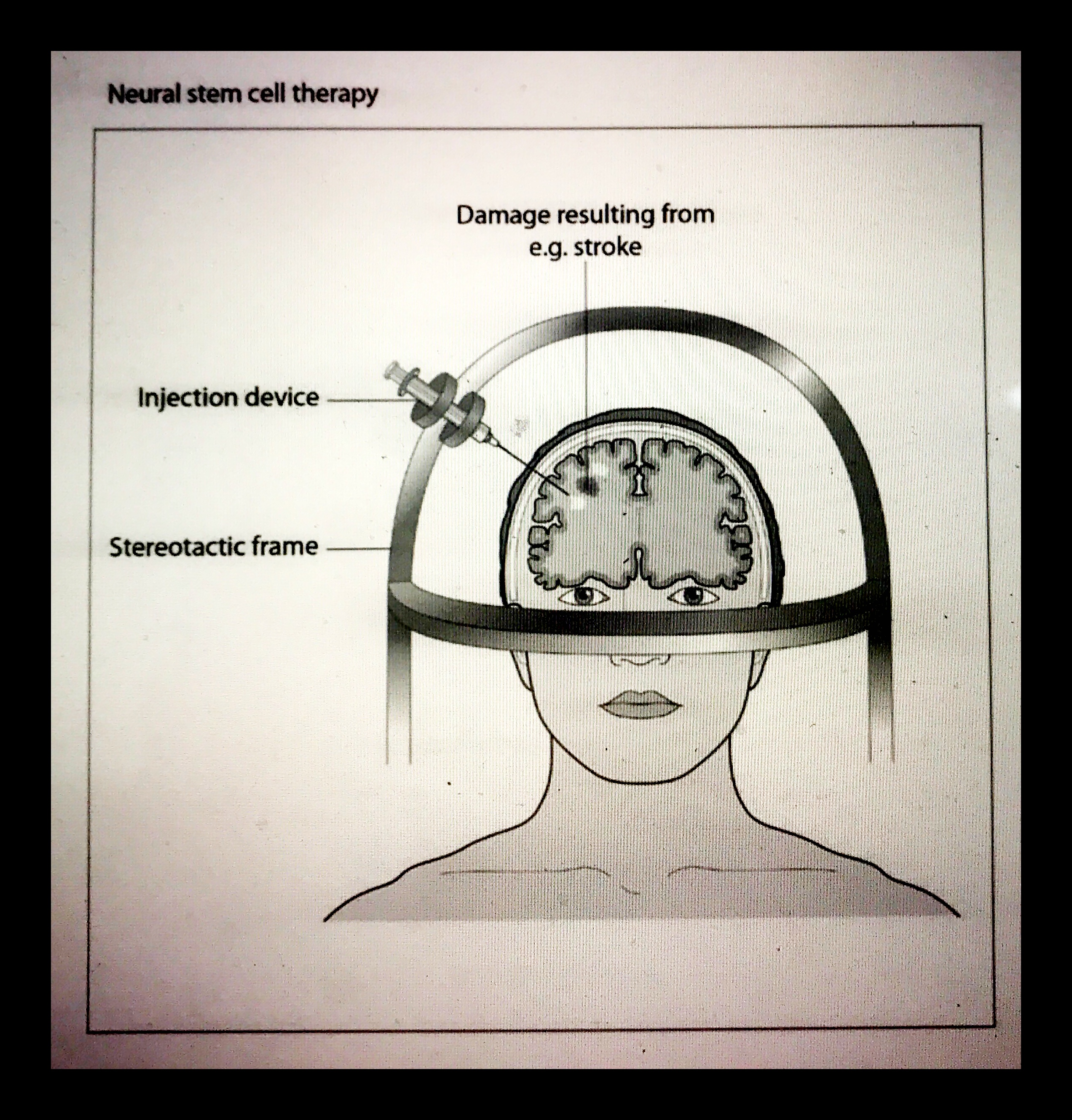
Product Description = Cerebracell is designed to stimulate true neurogenesis, the formation and nurturing of new neuron cells, to regenerate damaged or diseased brain tissue = true brain regeneration. We do this by bioelectric stimulation controlled release of more than 10 essential brain regeneration promotion cytokines. Our most important controlled cytokine release is SDF-1 which is a stem cell homing factor which recruits stem cells from a patient’s own bone marrow, fat and circulating blood to the stimulated brain tissue areas. We have another signal of opposite polarity for controlling the differentiation of those recruited stem cells into healthy functioning brain tissue. We also stimulate the release of IGF-1 for DNA level repair, HGF, EGF, Activin A+B, eNOS, VEGF, Follistatin and Tropoelastin all of which contribute to regeneration. eNOS, HGF and VEGF help improve blood supply to the treated area. For severe brain damage recovery and difficult disease cases we add our programmable micro infusion pump which is filled daily or weekly with our proprietary CCA-15 and CCR-15 fifteen component angiogenic and regeneration compositions comprised of a variety of cell types, growth factors, nutrient hydrogel, exosomes, Micro RNAs, brain matrix and other neurogenesis promoting molecules including harmine and tetrahydroharmine alkaloids and inflammation control agents. We believe that our combination bioelectric regeneration stimulator, micro infusion pump and proprietary 15 component angiogenic + regeneration compositions have the potential to do a better job of helping people recover from brain injuries or brain related diseases than any other therapy brought forward before. We are on a path to implement well designed clinical trials to prove this out.
For brain tumor cancer patients we have patent pending specially tuned bioelectric signals designed to stop cell division and blood supply to the tumors.

CerebraCell Milestones
46AD
Electric fishes used do treat headaches – Scribonius Largo, physician of the Roman emperor Claudius, in his text “Compositiones medicamentorum”
1804
Giovanni Aldini (1762–1834), nephew of the discoverer of animal electricity Luigi Galvani (1727–1798) and professor of Physics at the University of Bologna, performed electrical stimulations on the exposed human cerebral cortex of recently decapitated prisoners. In 1804, Aldini reported that cortical stimulation evoked horrible facial grimaces. This finding led him to conclude that the cortical surface could be electrically stimulated; supporting that electricity could have therapeutic effects in the treatment of many neuropsychiatric disorders (Aldini, 1804; Boling et al., 2002; Parent, 2004). Aldini’s experimentations and hypotheses led to direct research into two strands that would later developed during the ninetieth and twentieth century: on the one hand the use of brain stimulation for neurophysiologic investigation (initially on animals and then on humans) to understand the functioning of the brain, on the other hand the use of the techniques of brain stimulation for therapeutic purposes.
1809
Luigi Rolando (1773–1831) first used galvanic current to stimulate the cortical cortex of animals (Rolando, 1809), highlighting the functions of brain area.
1887
More precise and systematic observations on the topography of the brain had been made in 1887 by the British surgeon Victor Horsley (1857–1916) (Vilensky and Gilman, 2002)
1929
The discovery of electroencephalography (EEG) in 1929 by the German psychiatrist Hans Berger was a historical breakthrough providing a new neurologic and psychiatric diagnostic tool at the time. Galvani’s accidental discovery of “biological electricity” led to Volta’s discovery of the battery (voltaic pile). Using it, Rolando was the first to stimulate cerebral surface. Thus, enabling Fritsch and Hitzig and Ferrier to develop the idea of cerebral localization (Jackson, Gowers, Gotch and Horsley). It was understandable that brain electrical stimulation produces contralateral motor response, but it was unknown whether there was a spontaneous (intrinsic) brain electrical current that could be recorded. Caton was the first to report on the “current in the brain gray substances onto open brain. Based on Caton’s discovery and of those of Beck, Danilevsky, Prawdicz-Neminsky and others, Berger made the first EEG (electrocorticogram) recording on July 6, 1924, during a neurosurgical operation on a 17-year-old boy, performed by the neurosurgeon Nikolai Guleke. He reported on the topic in 1929, using the terms alpha and beta waves. The “spike and waves” (Spitzenwellen) were described shortly thereafter by the American group of EEG pioneers (H. and P. Davies, F. and E. Gibbs, Lenox and Jasper), although Berger had also observed them but considered them artifacts. The discovery of electroencephalography was a milestone for the advancement of neuroscience and of neurologic and neurosurgical everyday practice, especially for patients with seizures.
1938
Electroshock, introduced by Ugo Cerletti (1877–1963) was the first modern example of therapeutic application of brain stimulation for the treatment of severe psychosis (Cerletti, 1940; Kalinowsky, 1986). The application of an electric current on the skull evoked an epileptic seizure that “roughly” remodeled the neural connections, providing a clinical improvement to the patients.
1947
In 17 Ernst Spiegel and Henry Wycis, modifying the original apparatus of Clarke and Horsley (1906), produced the first human stereotactic frame that using pneumoencephalogram allowed to determine Cartesian coordinates of structures around ventricles (basal ganglia) for identifying the precise localization of the targets that had to be destroyed by radiofrequency (Spiegel et al., 1947; Zonenshyn and Rezai, 2005). Intra-operative electrical stimulation of these structures was systematically used for the exploration and the localization of the deep cerebral nuclei and for confirming target (Guiot et al., 1961; Gildenberg, 2005). These observations led to suggest that these stimulations of deep cerebral nuclei could be used not only as a method for diagnostic purposes but also as a therapeutic method itself. Thus, the evolution from lesional to stimulating functional neurosurgery was determined (Porta and Sironi, 2009).
1950
Fundamental studies of the neurosurgeon Wilder Penfield (1891–1976) were published – before the brain stimulation of the human cortex could give a real accurate representation of the human brain functions, including motor and somatosensory areas (cortical homunculus; Penfield and Boldrey, 1937; Penfield and Rasmussen, 1950).
1950
Brain stimulation for pain control, used as early as 1950 with good effects through temporary electrodes implanted into brain regions, after a first experimental phase, found its explanation in the “gate control theory” developed by Melzach and Wall in 1962 (Rezai and Lozano, 2002). These previous studies were the basis that led to the development of new techniques of neurostimulation: transcranial magnetic stimulation, cortical brain stimulation, and deep brain stimulation (DBS).
1950's
The origins of this technique are linked to the discovery of the effects of electrical stimulation of the deep brain areas, conducted during the stereotactic lesional functional neurosurgery to identify the correct position of coagulant electrodes for the treatment of dyskinetic disorders and tremor in Parkinson’s disease (Schwalb and Hamani, 2008). Thanks to the spread of stereotactic method, various studies demonstrated that, while “low-frequency stimulation” (5–10 Hz) could enhance tremor and other correlated symptoms, “high-frequency stimulation” (50–100 Hz) resulted in a reduction of symptoms (Albe Fessard et al., 1963; Blomstedt and Hariz, 2010). The pioneers of DBS were Delgado et al. (1952), Bekthereva et al. (1963), Sem-Jacobsen (1965), and Cooper (1978). Deep electrical stimulation of brain structures was originally introduced as a therapeutic option to treat behavioral disorders or chronic pain.
1952
The Spanish neuroscientist José M. Delgado, basing on his experience of deep neurophysiologic electrical stimulation in animals, first described the technique of implantation of intracranial electrodes in humans, indicating the importance of this method for diagnosis and its possible therapeutic role in patients with mental disorders (Delgado et al., 1952
1963
The first to use chronic depth stimulation as a therapy in motor disorders was Natalia Petrovna Bekthereva, neuroscientist at the Institute of Experimental Medicine and the Academy of Medical Sciences in Leningrad. In 1963 she published a work on the use of multiple electrodes implanted in sub-cortical structures for the treatment of hyperkinetic disorders (Bekthereva et al., 1963). However, since her papers were written in Russian, her works were not well known around the world. In her “therapeutic electro-stimulation,” as she named this method, she used “electric stimulation with high-rate pulses of suprathreshold current,” achieving excellent results (Bekthereva et al., 1975).
1965
Dr. Jose Manuel Rodriquez Delgado of Spain demonstrates ability to control behavior aggressiveness of bulls with brain implant.
1965
The Norwegian neurophysiologist and psychiatrist Carl Wilhelm Sem-Jacobsen initially used depth electrodes implanted for recording and stimulation in patients with epilepsy and psychiatric disorders. He successfully implanted multiple electrodes in the thalamus to stimulate the targets in order to identify the best lesional site in Parkinson’s disease. These electrodes were often left into the patient’s brain for several months, without any side effects. As he wrote: “these electrodes could then be used, following stimulation responses, to make incremental staged lesions in the target area” (Sem-Jacobsen, 1965, 1966; Blomstedt and Hariz, 2010).
1969
Dr. Delgado implanted electrodes in 25 human subjects, most of them schizophrenics and epileptics. In 1969 he described his brain stimulation researches and discussed critical aspects and ethic implications in the book Physical Control of the Mind: Toward a Psychocivilized Society, where he showed the tremendous opportunities but also the great risks derived from neurotechnology (Delgado, 1969).
1977
The experience of the American neurosurgeon Irving S. Cooper in placing electrodes over the cerebellum and into the deep thalamic nuclei for central palsy, spasticity and epilepsy was more extensive and continuous. In 1977 he reported its excellent results from chronic cerebellar stimulation in over 200 patients (Cooper, 1978).
1982
Leonhardt Ventures formed originally as H.J. Leonhardt & Co. the commercialization arm of inventor Howard J. Leonhardt.
1985
Dr. Robert O. Becker published landmark book The Body Electric.
1988
Leonhardt research team members Dr. Race Kao and Dr. George Magovern complete first first cases of large animal organ repair with stem cells published in 1989 in The Physiologist.
1988
Leonhardt forms World Medical Manufacturing Corporation in Sunrise, Florida to develop and commercialize cardiovascular organ monitoring, regeneration and recovery devices.
1993
Levin, Michael, Ph.D (now a part time consultant to Leonhardt’s Launchpads and CerebraCell) publishes Current and potential applications of bioelectromagnetics in medicine, (1993), ISSEEM Journal, 4(1): 77-87 laying the foundation of modern bioelectric regeneration research and goes onto to publish over 50 papers on the subject.
1995
Leonhardt leads team in Australia with Dr. Ken Thomson and Dr. Peter Field that completes first non-surgical repair of an aortic aneurysm clinically.
1998
Leonhardt research team collaborator Dr. Doris Taylor published study in Nature Medicine on myoblast cell repair of an animal heart.
1999
Leonhardt research team collaborator Dr. Shinichi Kanno publishes in CIRCULATION the Journal of American Heart Association first paper on bioelectric limb regeneration via controlled expression of proteins such as VEGF.
2000
Howard Leonhardt begins filing series of patents for organ regeneration based on bioelectric stem cell homing, proliferation and differentiation control, controlled protein expressions and in some cases combined with repeat deliveries of stem cells, growth factors, nutrient hydrogel and other organ regeneration promoting patents.
2001
Leonhardt leads team that completes first ever non-surgical stem cell repair of human heart in The Netherlands with Dr. Patrick Serruys. Team went on to complete, publish and present Pilot, Phase I, Phase II and Phase II/III study results working with 33 centers in the USA and 6 centers OUS. 84% of treated patients improved or did not decline. Only 16% of treated patients declined. 69% of control or placebo patients in these same studies worsened in heart function.
2007
Howard Leonhardt and noted bioelectric regeneration research Dr. Jorge Genovese formerly from the University of Utah join forces as co-inventors and begin filing numerous patent application claims together for bioelectric based organ regeneration and recovery.
2011-2016
Leonhardt team leads stem cell and bioelectric limb salvage studies with partners in Czech Republic, Switzerland, Germany and Mexico with 70 patients participating with successful results. Of 70 patients treated 66 legs were saved from amputation.
2015
CerebraCell is formed to develop a combination bioelectric stimulation + micro infusion pump + mixed stem cell & growth factor composition for brain regeneration with an initial focus on stroke, traumatic brain injury and brain cancer recovery. Dr. Leslie Miller joins Leonhardt’s Launchpads and Leonhardt Ventures as Chief Medical Officer. Former Chair of Dept. of Cardiovascular Medicine at University of Minnesota for over a decade. He helps oversee CerebraCell’s pre-clinical and clinical developments. Dr. Giorgio Lofrese and colleagues in Italy publish on the importance of IGF-1 in brain injury recovery – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4568328/ Kelsie Fortner Leonhardt Neuro Scientist, (B.S. Neuroscience) from Westminster College Utah joins CerebraCell founding team as an advisor and co-grant writer. Jeremy Koff experienced builder of Neuro Modulation startups joins CerebraCell’s Board of Directors and team as VP of Business Development. He is nephew of noted Neuro Modulation industry leader Alfred Mann that had more than $15 billion in exits during his career. Jeremy worked for more than 20 years under the mentorship of Alfred Mann in his companies.
2016
Leonhardt and Genovese filed provisional patent application for bioelectric stimulation controlled release of IGF-1. Leonhardt’s Launchpads Utah, Inc. with CerebraCell are accepted into the BioInnovations Gateway USTAR laboratory in Utah with access to over $30 million of research lab equipment and resources and subsidized research lab space. CerebraCell Utah lab team lead by Michael Angerbauer tests out various brain helmet designs for brain stimulation. Christian Oveson joins Utah lab research team. Leonhardt and Genovese filed provisional patent application for CerebraCell “Brain Saving Helmet”. Stanford team (not associated with CerebraCell) led by Dr. Gary Steinberg published landmark study demonstrating remarkable recovery of some brain stroke patients treated with modified stem cells. Dr. Thomas Ichim joins CerebraCell as senior advisor. Leading stem cell researcher from San Diego. Dr. Dinesh Patel joins Board of Director of Leonhardt’s Launchpads Utah, Inc. Noted biomedical entrepreneur and early stage life science angel investor. CerebraCell announces collaboration with HeartScore to develop a total stroke management program. CerebraCell presents at Neuro Tech Leaders Forum. Christian Oveson and Joshlyn Morgan join Utah lab research team. David Robinson, Devin Thorpe, Dr. Harrison Lazarus, Scott Marland, Dr. John Langell all join Leonhardt’s Launchpads Utah, Inc. Advisory Board. CerebraCell team meets with Bryan Johnson of Kernel to discuss potential research collaboration on cognitive function improvement. Leonhardt team creates new CerebraCell unit focused on this area called CerebraCell Brain-N-Hance.
2017
Leonhardt and Genovese file new series of patents focused on organ regeneration with combination therapies including brain regeneration. Asli Gozoren joins Leonhardt’s Launchpads as Director of Investor Relations. Dr. Santosh Kesari Director of Research at the Pacific NeuroSciences Institute in Santa Monica, CA joins CerebraCell as Chief Medical & Scientific Advisor. MIT team reports wireless deep brain stimulation – “Traditional deep brain stimulation requires opening the skull and implanting an electrode, which can have complications. Secondly, only a small number of people can do this kind of neurosurgery,” says Ed Boyden, an associate professor of biological engineering and brain and cognitive sciences at MIT, and the senior author of the study, which appears in the June 1 issue of Cell. CerebraCell team reaches out to them to try to initiate research collaboration. Dr. Warren Merrifield joins CerebraCell as Chief Technology Officer. Kapil Sharma and Sejal Chaudhari join Utah research lab team.
